Emergencies and disasters create stressful situations that can exacerbate ongoing behavioural health issues. Veterinarians have been identified as a professional group at elevated risk for behavioural health issues when they are involved with an emergency response. Prior studies looking at transboundary animal disease disaster management demonstrate the significant and long-lasting mental health effects experienced by veterinary responders. To examine the scale and scope of behavioural health issues exhibited by veterinary responders, an online and anonymous survey was conducted with veterinarians who had participated in events in the Asia-Pacific, Africa, Europe, Latin America and North America regions. The results of the survey showed that behavioural health issues were reported by 51 per cent of respondents during and up to 6 months after the disaster. Behavioural health issues reported included loss of sleep, anxiety, difficulty with personal and professional relationships, mood swings, depression, nightmares and flashbacks and suicidal thoughts. The scope and magnitude of veterinarians with behavioural health issues associated with disasters underscores the need for guidelines, standards, education, training and further research in this area.
Introduction
Emergencies and disasters can have impacts on human, animal and environmental health. The psychological or behavioural health effects on veterinary responders across disaster types has not been widely studied. The aim of this research is to examine the scale and scope of behavioural health issues exhibited by veterinary responders.
A ‘disaster’ is ‘A serious disruption of the functioning of a community or a society at any scale due to hazardous events interacting with conditions of exposure, vulnerability and capacity, leading to one or more of the following: human, material, economic and environmental losses and impacts’ (UNDRR n.d.). Mental health, psychological health and behavioural health are terms that have been used interchangeably. For this study, the concept of behavioural health is used as described in Behavioral Health vs Mental Health Alvernia University 2021: ‘Behavioral health describes the connection between behaviours and the health and wellbeing of the body, mind and spirit’. This concept includes how behaviours effect physical and mental health.
Because disasters have significant impacts on human and animal health, economies, trade and societies, animals and animal-related issues are increasingly becoming part of disaster management and risk reduction planning due to economic, health, welfare and social aspects. The United Nations Office for Disaster Risk Reduction Annual Report 2019 (UNDRR 2020, p.12) estimated the global economic losses from natural hazards at USD$232 billion, highlighting the animal component of disasters by citing Australia’s October 2019 to March 2020 bushfires that killed an estimated 1.25 billion animals.
The World Organisation for Animal Health (OIE) disaster preparedness and response guidelines (OIE 2016) as well as the United Nations Food and Agriculture handbook, Good Emergency Management Practice: The Essentials (GEMP) (Honhold et al. 2011), have identified critical roles for veterinarians in emergency management including the protection of animals, people and economies. For example, veterinarians are critical during a transboundary disease outbreak, which is a specific animal-disaster category that can cause significant economic, trade and food security risks at national and international scales (Otte, Nugent & McLeod 2004). Transboundary animal disease control is a process that mitigates these negative effects. Examples include the 2001 foot-and-mouth disease outbreak in the United Kingdom (Davies 2002) and the 2017 avian influenza outbreak in the USA (Lee et al. 2017). In both cases, part of the control measures included depopulation or killing of diseased and healthy animals within a geographic area to prevent the spread of the disease and to protect the remaining livestock. Veterinarians participate in depopulation at all levels including the decision process, supervision of depopulation and killing of designated animals. The psychological effects of killing diseased and healthy animals has been described as ‘perpetration-induced traumatic stress’ (Whiting & Marion 2011). Depopulation has behavioural health effects on the communities, producers and those undertaking depopulation.
Veterinarians have been identified as having a potentially high rate of suicide as well as other behavioural health issues. Studies in the USA show that veterinarians may have a proportionate mortality rate from suicide of 1.7 to 2.6, being 3 times that of the general population (Tomasi et al. 2019). Nett and co-authors (2015) indicated 9 per cent of veterinarian respondents to their survey reported current serious psychological distress. These studies highlight the background behavioural status of veterinarians. Khatri, Fitzgerald and Meen (2019) provided a systematic review of published articles on health risks for disaster responders that showing mental health as a key issue. Forty-five of the 71 identified articles cited in the review included veterinarians as responders, however, there is a general lack of detailed information on veterinary responder behavioural health. The combination of underlying veterinary behavioural health issues and the added stresses of a disaster response creates an environment for elevated behavioural health risks.
Veterinary psychological or behavioural health stress in emergency response has been associated with specific transboundary disease disasters. Despite the reports on this issue there are very few references to behavioural health in international animal health standards and guidelines. The Terrestrial Animal Code (OIE 2019) has numerous references to animal welfare, but it does not address human welfare to a significant extent. The UNFAO GEMP identifies psychological distress support needs by producers and communities, but it gives limited attention to responders (Honhold et al. 2011). These high-level references provide guidelines for the technical aspects of veterinary emergency response and do not address the safety, health and wellbeing of veterinary responders.
Nusbaum, Wenzel and Everly (2007) identified the need for psychological first aid for both veterinary responders and the animal-owning population. A study of the behavioural health effects for veterinarians participating in the foot-and-mouth disease response in the Netherlands in 2001 showed the potential long-lasting consequences with 40 per cent of veterinarians showing signs of traumatic stress after 6 years (Noordman & Endenburg 2008). Similarly, posttraumatic stress disorder (PTSD) was identified by Hibi and co-authors (2015) in veterinary personnel 2 years after the foot-and-mouth disease control program in Japan in 2010. However, there is a lack of programs available or in use to address behavioural health of veterinarians (Wasson & Wieman 2018). The United States Department of Agriculture (USDA) National Animal Health Emergency Management Systems (NAHEMS) along with the Center for Food Security and Public Health has published guidelines for addressing responder behavioural health in animal disease events as one model (CFSPH 2018). But the training, exercising, execution and evaluation of these guidelines during actual events has not been examined. Documentation of veterinary behavioural health issues associated with disasters has primarily focused on the responses to transboundary disease in specific countries. The broader range of behavioural health issues in a variety of disasters and locations is worthy of study. Therefore, a study of behavioural health of veterinarian responders to qualify and quantify the scale and scope of behavioural health issues should be across identified disasters events including conflict, technological disasters, natural hazards including the subcategory of disease events as well as geographic locations.
Method
A cross-sectional study was conducted via an online anonymous survey consisting of 24 questions. The survey was developed, tested for functionality and reviewed by veterinarians, disaster responders and behavioural health practitioners for validity before data collection on the Qualtrics® platform. Questions were in pick-list and free-text formats. The purpose of the survey was to identify the scope and scale of behavioural health issues of veterinarians responding to disasters. In addition to informed consent language, the survey included stress warnings for participants to stop the survey and seek support if feeling distressed. A link to the survey was sent to individuals identified as veterinarians from contact lists of the OIE headquarters and attendees from conferences with a focus on disaster and emergency management. Supporting this snowball sampling approach, the survey link was coded for reuse so it could be forwarded to others. Two seeding emails announcing the survey were sent; the first with 1113 email addresses and the second, one month later, with 968 email addresses that were determined to be active. The survey was open for one month following the second notice. The results were tabulated and analysed by the authors.
The research received ethical review and approval before the survey was fielded and was conducted under Institutional Review Board #875 V.0, Lincoln Memorial University.
Survey results
There were 255 responses to the survey. Of these, 15 responses were discarded as they did not meet the criteria for inclusion, resulting in 240 useful responses. Criteria for inclusion were agreement to participate, responding to the 4 independent variable questions (number of disasters participated, number of years practicing as veterinarian, birth year and gender) and agreement that the respondent participated in at least one disaster and identification of the region where the disaster event occurred. Not every respondent answered each question resulting in an 89 per cent (227/255) full completion rate. The organisational affiliation of the respondent was not identified in the survey therefore government, private and non-government roles of responding veterinarians were not determined. The non-probabilistic data collection technique limits the results to descriptive statistics. These results reflect responses to individual questions and are rounded to nearest whole numbers.
Most respondents (73%, 174/240) had participated in 2 or more disaster events with over a third (35%, 85/240) participating in 4 or more events. Respondents were equally distributed by gender (male 53%, 126/240 and female 48%, 114/240) and the majority (85%, 205/240) had worked for more than 10 years as a veterinarian. The responses covered disasters that occurred in Canada and the USA (40%, 96/240), Europe (31%, 75/240), Asia-Pacific (12%, 28/240), Africa (11%, 26/240) and Latin America (6%, 15/240). More than half of the respondents had participated in an animal disease outbreak (52%, 124/240) with natural hazards the second highest reported (36%, 87/240) followed by military or civil conflict (6%, 14/240), human disease (4%, 9/240) and technological disasters (3%, 6/240). More than half the respondents (54%, 129/239) reported participating for 5 or more weeks during the disaster.
Veterinarians described multiple response roles with the majority in fieldwork (45%, 108/239) and emergency operations centres (29%, 69/239) and the remaining equally divided between categories of epidemiology, laboratory and other. Those working in fieldwork served in a variety of roles with most (88%, 95/108) tasked with depopulation, carcass management and quarantine tasks.
Many respondents (60%, 142/237) were unaware of current standards, guidelines or standard operating procedures for their behavioural health. Few respondents reported receiving training before deployment (24%, 56/238) or during deployment (26%, 61/238), much less behavioural health support during (16%, 38/234) or after (13%, 31/234) the event. However, 51 per cent (120/235) reported experiencing at least one behavioural health symptom during the disaster response and 34 per cent (77/227) of respondents reported at least one behavioural health symptom after the disaster.
Survey analysis
Several veterinary behavioural health issues were identified during and after responding to an emergency with half of respondents reporting behavioural health symptoms (see Figure 1). These responses included a variety of behavioural health symptoms ranging from sleeplessness and anxiety to depression and thoughts of suicide. In addition, these symptoms often persisted 6 months after a deployment with several of the most significant symptoms (mood swings, depression, nightmares and suicide thoughts) showing little change from numbers reported during the disaster.
Figure 2 illustrates the behavioural health issues reported across the spectrum of disasters including transboundary disease disasters, human disease, conflict, natural and technological disasters. Figure 3 shows that males and females equally reported experiencing behavioural health symptoms. Figure 4 shows that behavioural health issues were reported in every geographic area surveyed.
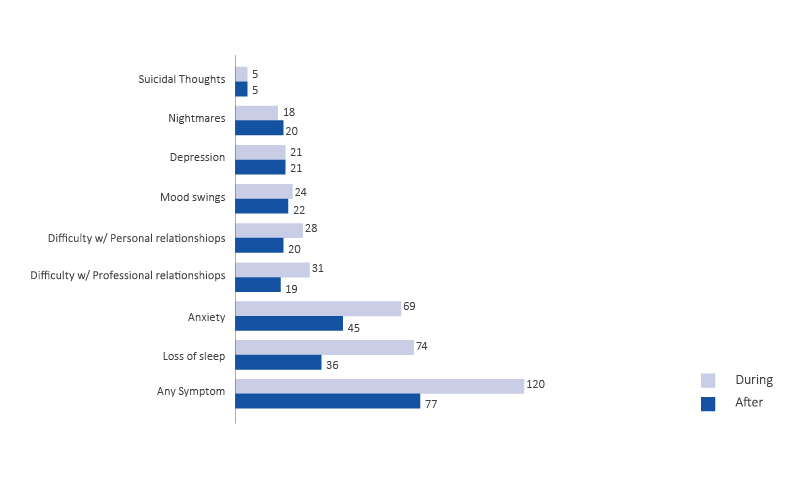
Figure 1: The numbers of reported behavioural health issues experienced during the disaster response and 6 months after the disaster response by symptom type (n=240).
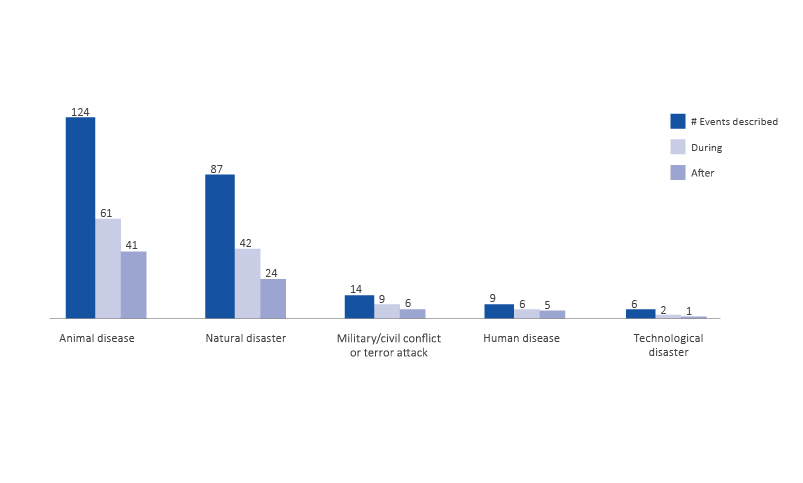
Figure 2: The numbers of reported behavioural health issues experienced during the disaster response and 6 months after the disaster response by disaster type (n=240).
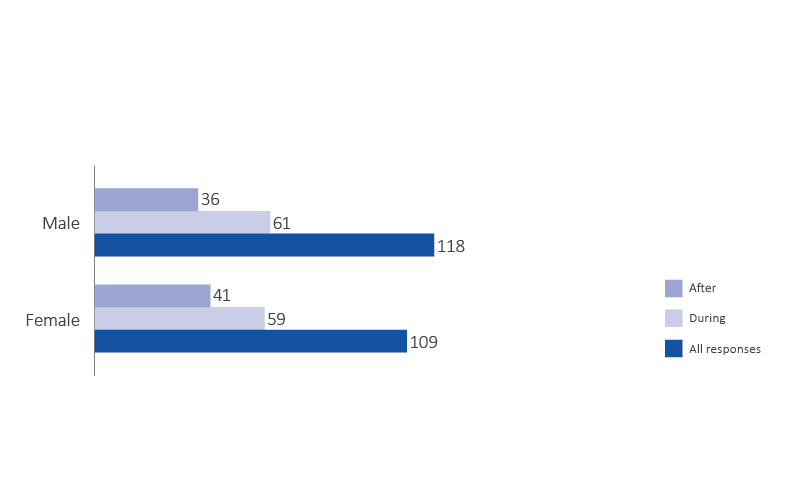
Figure 3: The numbers of reported behavioural health issues experienced during the disaster response and 6 months after the disaster response by male and female respondents (n=227).
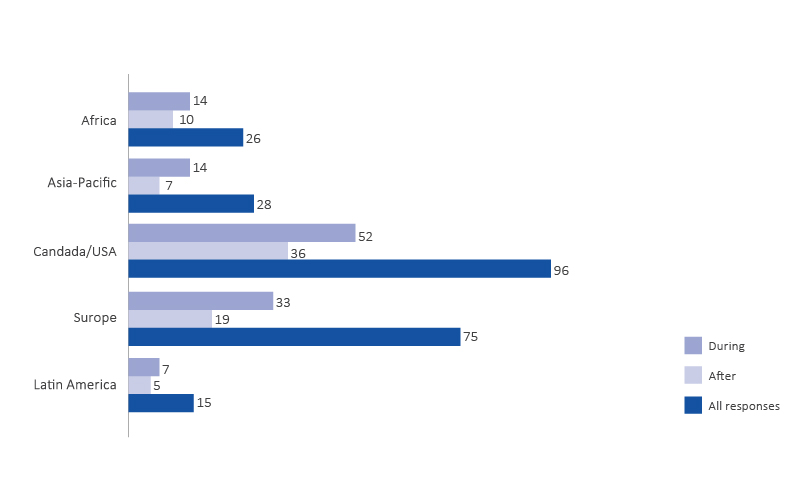
Figure 4: The numbers of reported behavioural health issues experienced during the disaster response and 6 months after the disaster response by region (n=240).
Behavioural health training and education for responders before a disaster event was generally reported as lacking or insufficient. Similarly, behavioural health support during and after the response was reported as ‘highly variable’. Few guidelines, standards and operating procedures for behavioural health are available and are not consistently published. When examples of mitigation techniques such as time off and swapping of duties were reported, their execution was highly variable.
The survey asked an open-ended question: ‘What behavioural health support do you believe veterinarians need BEFORE, DURING and/or AFTER participating in a disaster event? A total of 195 respondents made 186 suggestions and 3 languages were used. The suggestions were separated, coded and sorted. Changes in behavioural health training and processes before, during and after deployment were highlighted. For example, there was a recommendation for briefings that prepare veterinarians for:
A clear, even if hard to see/hear, picture of what they will see and experience during deployment. That can include scenes of depop [animal depopulation]; interviews and retrospectives of other DVMs [doctors of veterinary medicine] and producers. The sights (and smells) of carcasses.
The need to communicate situational awareness, provide time off to rest during the event and personal time off after the event to recover before returning to regular duties was reported:
Broad resilience training before, time off during and after-event assessment to determine needs.
Respondents wrote about the need for guidance:
We need a standardised course before we deploy.
Leadership was cited as a need in the response to the question: ‘Awareness briefing, good leadership to mitigate risks, availability of counselling’. The need for counselling during the event was frequently mentioned:
Counselling is the most needed.
Fifteen respondents indicated behavioural health support was not required:
We in [named country] don’t need behavioural health support.
Several free-text comments were extensive and recounted health issues related to the veterinary role and profession experienced before, during and after participating in a response. An example:
Eventually I had a major depressive episode hospitalised 30 days back to work 6 months. May have had nothing to do with the event.
This comment highlights the severity of the effects as well as the complexity of specifically attributing participation in a disaster as a single triggering event for behavioural health effects.
Discussion
Biases in sampling is acknowledged and may have occurred through the selection of initial recipient emails, through providing the survey in English and through self-selection. Self-selection could have occurred as those with a behavioural health issue may have been more likely to respond and people may have forwarded the survey to others whom they knew or suspected suffered behavioural health events. However, this is balanced by reaching a ‘hidden’ community of veterinarians who have participated in a disaster event and may have suffered behavioural health symptoms and not been sent the survey. The small sample size precludes definitive statements on behavioural health issues for veterinarians. However, the responses provided and the criticality of this topic is sufficient information to identify potential areas of concern and a starting point for further research.
The scope of behavioural health issues in the study was reported across the geographical areas surveyed indicating it is a widespread issue. Respondents’ behavioural health issues were noted in all the categories of emergencies presented in the survey. This indicated that symptoms were not limited to transboundary disease responses. Behavioural health issues were also experienced equally across genders indicating that there was not a gendered difference. These results suggest that behavioural health issues are expanded across a wide range areas, genders and disaster types.
The scale of behavioural health issues in the study was that 50 per cent of respondents reported symptoms during the response and 32 per cent reported still having symptoms 6 months later. This suggests there is a high level of behavioural health issues associated with disaster response. Not all the behavioural health issues described are due to the stress and trauma of the event. Nett and co-authors (2015) describe the background level of behavioural health issues experienced in the veterinary profession and that these may be represented in the responses provided. However, the number and range of behavioural health symptoms reported suggests that behavioural health is a significant responder wellness issue. This was reflected in the free-text comments. An additional issue identified was the lack of awareness of standards, guidelines and operating procedures that prevent, mitigate or treat behavioural health effects. There was minimal reported training and behavioural health support during or after the event.
The responses in this survey were consistent with other studies on disaster responders that cited PTSD in multiple events. Australian volunteer firefighters exhibited PTSD at 32 per cent at 4 months post event (Bancroft 2019, Naushad et al. 2019) and a Western Australia report stated that 10 to 30 per cent of responders were at risk of developing PTSD (Western Australia Legislative Assembly 2012). In recognition of this issue, Phoenix Australia published a Guide for Firefighters with Posttraumatic Stress Disorder (Phoenix Australia Centre for Posttraumatic Mental Health 2013). Nurses responding to Hurricane Katrina reported 20 per cent with PTSD and depression was reported at 19 per cent in World Trade Center terror attack emergency medical service responders several years following event (Naushad et al. 2019).
Conclusion
This research used an online survey to garner 240 responses to identify a range of behavioural health issues experienced by veterinary responders. The survey considered large regions, all disaster types and gendered themes. Survey analysis indicated that the scale and scope of veterinary responders’ behavioural health issues are significant and the findings indicate that further study and action to improve health outcomes is warranted.
Actions to address the behavioural health issues of veterinarians in disaster response:
- OIE, in conjunction with UNFAO, develop guidelines and standards for veterinary behavioural health training, education and monitoring and incorporate these into documents such as the Terrestrial Animal Health Code, GEMP and OIE guidelines.
- OIE incorporate behavioural health programs into standards for the provision of veterinary services.
- National veterinary services in each country incorporate behavioural health training, education and processes into disaster preparedness and response programs.
- National veterinary services establish and execute protocols and resources to support veterinary responders before, during and after responses.
- National veterinary services develop and implement reporting and assessment protocols and procedures for health and wellbeing.
- Professional organisations promote veterinary behavioural health as a critical issue and educate their members and stakeholders.
- Veterinary training in veterinary curricula and continuing education settings need to address behavioural health for veterinarians who may be called on to take on the responder role.
- Research funding to understand the underlying risk factors for responders, best practices to build resilience, best practices for responder support and mechanisms to mitigate behavioural health risks associated with disaster response. This research should include all animal responders such as veterinary technicians and nurses, administrative and support personnel and volunteers as well as communities and individuals.
This research provides evidence for the significant scale and scope of behavioural health risk for veterinarians responding to emergencies. To address this will take focus, effort and action by the veterinary profession to protect its members.


